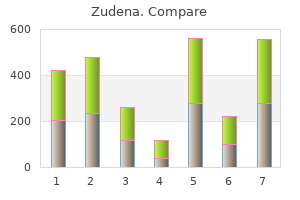
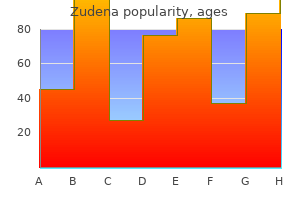
Zudena"Buy zudena 100mg low price, erectile dysfunction after age 40". By: S. Dawson, M.A., M.D., M.P.H. Clinical Director, Drexel University College of Medicine If complete transection has occurred or a urethral catheter cannot be placed why smoking causes erectile dysfunction zudena 100mg on-line, the patient can be taken to the operating room, where a suprapubic cystotomy tube is placed. An antegrade-retrograde two-team approach using cystoscopy and fluoroscopy is then performed in an effort to place a catheter across the defect. Recent literature has suggested that early realignment decreases the need for subsequent urethroplasty without compromising erectile or sphincter function. However, if a primary realignment is not feasible, a suprapubic catheter is used for drainage, and delayed repair (3 months after the injury) is indicated. A progressive perineal anastomotic repair in these cases has a success rate of more than 95%. Epithelializing stent for benign prostatic hyperplasia: A systematic review of the literature. Dorsal onlay buccal mucosa versus penile skin flap urethroplasty for anterior urethral strictures: Results from a randomized prospective trial. Long-term followup for excision and primary anastomosis for anterior urethral strictures. Treatment of male urethral strictures: Is repeated dilation of internal urethrotomy useful Buccal mucosa graft urethroplasty for anterior urethral stricture repair: Evaluation of the impact of stricture location and lichen sclerosis on surgical outcome. The treatment of posterior urethral disruption associated with pelvic fractures: Comparative experience of early realignment versus delayed urethroplasty. Lichen sclerosis: Review of the literature and current recommendations for management. In male patients, other risk factors include prostate surgery and bladder outlet obstruction from an enlarged prostate. Although urgency incontinence is often idiopathic, lower urinary tract symptoms in general are common among people with neurologic disease such as multiple sclerosis, spinal cord injury, or spinal dysraphism. During the storage phase, the sympathetic and somatic nerves work in concert to keep the urethra contracted and the detrusor muscle relaxed, allowing urine to fill the bladder at low bladder pressures (the bladder has high compliance during storage). Once the voiding reflex is activated, sympathetic and somatic neural activity is diminished, resulting in relaxation at the urethral sphincter and pelvic floor, and parasympathetic activity increases via cholinergic neurotransmission, resulting in detrusor contraction and bladder emptying. Failure to store urine normally can manifest as urinary incontinence, urinary frequency, and/or nocturia secondary to bladder and/or urethral dysfunction. Alternatively, urine leakage can result from a nonurologic cause (functional incontinence) and can sometimes be reversible when the underlying cause is identified (Box 1). Stress incontinence occurs when increases in intraabdominal pressure overcome the ability of the urethral sphincter to stay closed. The patient complains of leakage with activity, cough, lifting, and other stressors. Stress incontinence can result from urethral neuromuscular injury, urethral vascular changes, or lack of proper pelvic floor support in some women with associated pelvic organ prolapse. Stress incontinence in a male patient is most commonly due to a radical prostatectomy performed for treatment of prostate cancer. Urgency incontinence is less well understood, but it can be due to uninhibited bladder contractions (detrusor overactivity) and can result in large-volume urine loss. It is unclear whether the etiology for urgency incontinence or "overactive bladder" originates in the central nervous system, the peripheral nervous system, or the bladder. In the neurogenic population, a poorly compliant bladder can develop, which results in a steady increase in storage bladder pressures that eventually results in leakage in addition to neurologically induced uninhibited bladder contractions (neurogenic detrusor overactivity). Bladder outlet obstruction or decreased bladder contractility can result in overflow incontinence due to incomplete bladder emptying. Bladder outlet obstruction can result from prostatic obstruction or bladder neck or urethral stricture in male patients and, less commonly, from advanced prolapse or as a side effect from surgical correction of stress incontinence in women. Prevention Because of the association of urinary incontinence with diabetes and obesity, it is likely that efforts to prevent these disease states would lower the incidence of urinary incontinence. Indeed, weight loss is an effective treatment option for urinary incontinence, and this has been demonstrated scientifically. Additionally, a behavioral modification program that included pelvic floor muscle training resulted in improved continence status in postmenopausal women in a randomized, controlled trial.
General supportive care includes administration of fluids to correct hydration and hypotension and correction of electrolyte abnormalities and acid-base imbalance erectile dysfunction injections treatment purchase 100 mg zudena amex. In case of hypomagnesemia, a loading dose of 2 g magnesium sulfate 10% is administered by intravenous solution over 5 minutes in the intensive care unit with blood pressure and cardiac monitoring and calcium chloride 10% on hand in case of overdose. Hemodialysis can be used in severe cases when conventional therapy is ineffective (rarely needed). Withdrawal is treated with hydration and large doses of chlordiazepoxide (Librium) 50 to 100 mg or diazepam (Valium) 2 to 10 mg intravenously; these doses may be repeated in 2 to 4 hours. Withdrawal can occur in presence of elevated blood ethanol concentration and can be fatal if left untreated. Chest radiograph is warranted to determine whether aspiration pneumonia is present. Onset is usually in 30 minutes but may be delayed by co-ingestion of food and ethanol. The half-life of ethylene glycol without ethanol is 3 to 8 hours; with ethanol, it is 17 hours, and with hemodialysis it is 2. The onset of manifestations is 30 minutes to several hours longer after ingestion with concomitant ethanol ingestion. Hypocalcemia, tetany, and calcium oxalate and hippuric acid crystals in urine can be seen within 4 to 8 hours but are not always present. Early, before metabolism of ethylene glycol, an osmolal gap may be present (see Laboratory Investigations). Later, the metabolites of ethylene glycol produce changes starting 4 to 12 hours following ingestion, including an anion gap, metabolic acidosis, coma, convulsions, cardiac disturbances, and pulmonary and cerebral edema. Because fluorescein is added to some antifreeze, the presence of fluorescence may be a clue to ethylene glycol exposure. However, it has been shown that fluorescent urine is not a reliable indicator of ethylene glycol ingestion and should not be used as a screen. After 12 to 36 hours, cardiopulmonary deterioration occurs, with pulmonary edema and congestive heart failure. Neurologic sequelae may occur rarely, especially in patients who fail to receive early antidotal therapy. Findings include facial diplegia, hearing loss, bilateral visual disturbances, elevated cerebrospinal fluid pressure with or without elevated protein levels and pleocytosis, vomiting, hyperreflexia, dysphagia, and ataxia. Urinalysis should look for oxalate ("envelope") and monohydrate ("hemp seed") crystals. A serum ethylene glycol concentration of 20 mg/dL is toxic (ethylene glycol levels are very difficult to obtain). Crossreactions with propylene glycol, a vehicle in many liquids and intravenous medications (phenytoin [Dilantin], diazepam [Valium]), other glycols, and triglycerides may produce spurious ethylene glycol levels. An increased osmolal gap is produced by the following common substances: acetone, dextran, dimethyl sulfoxide, diuretics, ethanol, ethyl ether, ethylene glycol, isopropanol, paraldehyde, mannitol, methanol, sorbitol, and trichloroethane. Although a specific blood level of ethylene glycol in milligrams per deciliter can be estimated using the equation below, this is not considered to be a reliable method and should not take the place of obtaining a measured ethylene glycol blood concentration. The toxic metabolites are not osmotically active, and patients presenting late may show signs of severe toxicity without an elevated osmolar gap. In the first few hours, the measured serum osmolality should be determined and compared to calculated osmolality (see osmolality equation, earlier). If seizures occur, one should measure serum calcium (preferably ionized calcium) and treat with intravenous diazepam. If the patient has hypocalcemic seizures, he or she should also be treated with 10 to 20 mL 10% calcium gluconate (0. Ethanol therapy should be initiated immediately if fomepizole (Antizol) is unavailable (see next paragraph). Ethanol should be administered intravenously (the oral route is less reliable) to produce a blood ethanol concentration of 100 to 150 mg/dL. The loading dose is 10 mL/kg of 10% ethanol intravenously, administered concomitantly with a maintenance dose of 10% ethanol of 1. The blood ethanol concentration should be measured hourly and the infusion rate should be adjusted to maintain a blood ethanol concentration of 100 to 150 mg/dL. Discount zudena 100 mg without prescription. Himalaya Himcolin Gel for Erectile Dysfunction | Customer Review | Ayurvedic product. Options include cystoscopy with placement of a ureteral stent to temporarily decompress the obstruction erectile dysfunction treatment honey buy generic zudena on-line, or placement of a percutaneous nephrostomy tube. Septic patients should be emergently decompressed with a ureteral stent or a nephrostomy tube. The decision to recommend a procedural intervention is often multifactorial, involving factors such as chance for spontaneous passage, absolute indications for intervention, and patient preference and work and family requirements. Ureteral stones larger than 1 cm have a minimal chance of passing and require surgical treatment in most cases. After ureteroscopy a ureteral stent may be left in place, which is generally removed in the office in 1 to 2 weeks. Stents are usually well tolerated, but some patients do experience bothersome urinary symptoms including urgency, frequency, and bladder pain at the end of urination. Percutaneous access is obtained by either interventional radiology or by the urologist, and a 30-F working tract is created. The calculus is then fragmented by ultrasonic or pneumatic lithotripsy devices, and fragments are removed. Clinical Manifestations Patients with renal calculi generally present for evaluation when the stone begins to move down the urinary tract. Acute renal or ureteral colic from an obstructive calculus is described as intermittent crampy pain that is severe and often debilitating. Some patients also experience nausea and vomiting during these episodes and can have varying amounts of blood in the urine. Patients with staghorn calculi can present with signs and symptoms of a systemic infection and are at risk for progression to sepsis. Diagnosis A thorough history should be taken during the initial evaluation, with questions focusing on the nature and location of the pain, radiation of the pain, duration of pain, and presence of nausea, vomiting, dysuria, and hematuria. Questions directly related to stone disease should be asked, such as personal or family history of stone disease, age of first stone, and history of recurrent urinary tract infections. If the patient has had prior stones, it is important to ask how the stone was managed, did it pass spontaneously or was an intervention required The physical examination usually demonstrates significant costovertebral angle or flank tenderness to palpation. Peritoneal signs are not common with renal calculi, and an alternative diagnosis should be pursued if these are found. Patients with fevers, tachycardia, or labile blood pressure and flank pain should be considered to have an obstructing stone and should be treated emergently. Laboratory and Radiographic Work-Up the typical work-up for a stone patient consists of laboratory studies, which include a comprehensive metabolic panel, complete blood count, urinalysis with microscopic analysis, urine culture, and pregnancy test for premenopausal women. Attention should be paid to the urinalysis for presence of crystals, hematuria, signs of infection, and pH. An elevated creatinine could indicate obstruction of the kidney or dehydration from nausea and vomiting. Initial imaging studies usually consist of a plain abdominal radiograph to examine for the presence and location radiopaque stones. These samples should be analyzed for urine volume, pH, calcium, creatinine, sodium, phosphate, oxalate, uric acid, citrate, and cystine levels. General recommendations to prevent recurrent stones include increasing water intake to make at least 2 L of urine per day and adhering to a low-salt, low-meat, moderatecalcium diet. Hypercalciuria is treated by thiazide diuretics (hydrochlorothiazide)1 25 mg daily and/or potassium citrate (Urocit-K) 10 to 20 mEq twice daily. Hyperoxaluria is treated by decreasing dietary intake of oxalate with oral calcium supplementation. Hyperuricosuria is treated by the addition of potassium citrate to increase the urinary pH plus allopurinol (Zyloprim) to decrease serum uric acid. Patients with cystine stones are best managed by a lowmethionine diet and alkalization of the urine with potassium citrate. If these measures are not sufficient, cystine binders such as tiopronin (Thiola) or D-penicillamine (Cuprimine) can help prevent recurrent cystine stones.
For the hemolytic anemias low testosterone causes erectile dysfunction generic 100mg zudena, examination of the bone marrow is seldom helpful and generally not necessary in the diagnostic process. A delayed transfusion reaction is often not appreciated but should be suspected when the hemoglobin level falls more quickly than expected following a transfusion. The diagnosis can be made by demonstrating a new serum alloantibody in the recipient of the transfused blood. A urine hemosiderin can also be positive, reflecting hemolysis that occurred several days previously. Congenital Hemolytic Anemias the diagnosis of congenital nonimmune hemolytic anemias is often suspected when the anemia is long-standing. A family history of anemia, splenectomy, or gallstones can also be a clue to a congenital process. The membrane disorders all have findings on the peripheral smear (see Table 1), though these findings are not necessarily specific to the disorder. A specialized test, osmotic gradient ektacytometry, can be used to help in diagnosing these disorders. A supravital stain, such as crystal violet, brilliant cresyl blue, or methylene blue, can demonstrate Heinz bodies. If the diagnosis is still suspected after obtaining a normal result, a repeat test 2 to 3 months after the acute hemolytic episode should be performed. Hemoglobin electrophoresis should be performed to diagnose a suspected hemoglobinopathy. The most common hemoglobinopathy causing hemolysis, sickle cell anemia, is readily diagnosed by this test. However, other hemoglobinopathies causing hemolysis, specifically the unstable hemoglobins, may be electrophoretically silent. If the diagnosis of an unstable hemoglobinopathy is suspected, a supravital stain can demonstrate Heinz bodies and a heat stability test should be obtained for definitive diagnosis. The peripheral smear is usually very helpful in diagnosing the acquired causes of nonimmune hemolytic anemias. The peripheral smear can also be diagnostic of certain infections (malaria, babesiosis). The diagnosis of paroxysmal nocturnal hemoglobinuria is made by flow cytometry using peripheral blood cells or bone marrow aspirate and the demonstration of deficiency of hematopoietic cell proteins normally linked to the anchoring glycosylphosphatidylinositol protein. Acquired Nonimmune Hemolytic Anemias the diagnosis of acquired causes of nonimmune hemolytic anemias is suspected when a hemolytic anemia is new in onset and previous hemoglobin levels have been normal. Even though the anemia 851 Differential Diagnosis the differential diagnosis of the hemolytic anemias includes the reticulocytosis that can be seen with correction of anemia due to replacement of a deficiency (iron, folate, vitamin B12) or recovery from bleeding. Approximately 80% of patients have a rapid response to corticosteroids, typically within 1 week after starting therapy. The majority of adult patients receive high-dose oral prednisone 1 mg/kg/day during the initial phase of treatment. Intravenous methylprednisolone (Solu-Medrol) may also be used at daily doses of 100 to 200 mg. Hemolytic Anemia 852 Once the hematocrit has increased, the dose should be decreased and subsequently tapered at a slow rate over several months. Patients who require more than 10 to 15 mg of prednisone daily to keep an adequate hematocrit or those who did not respond to the corticosteroids will need second-line treatment. Patients who are candidates for splenectomy should receive immunizations against encapsulated organisms at least 2 weeks before the procedure. Rituximab, given at a dose of 375 mg/m2 weekly for 4 weeks, results in an overall response rate of 82% with many sustained responses. Recently described is the use of a lower dose of rituximab, 100 mg, weekly for 4 weeks. For cases refractory to steroids, splenectomy and rituximab may respond to other immunosuppressive therapies such as cyclophosphamide (Cytoxan), azathioprine (Imuran),1 or cyclosporine (Neoral). Other treatment options that have been used with some success include danazol (Danocrine)1 and plasmapheresis.
|