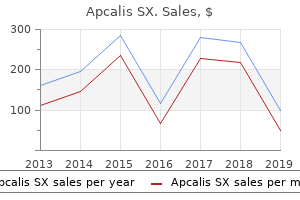
Apcalis SX"Purchase apcalis sx 20mg without a prescription, over the counter erectile dysfunction pills uk". By: B. Redge, M.A.S., M.D. Associate Professor, Touro College of Osteopathic Medicine The outcome of laparoscopic myotomy and hemifundoplication has been well documented erectile dysfunction treatment levitra purchase apcalis sx on line. Richter and coworkers reviewed published reports to date, including 254 patients with an average success rate of 93% at 2. Intraoperative complications consist largely of mucosal perforation, and have been more likely to occur after botulinum toxin injection. The incidence of objective reflux disease as evidenced by abnormal acid exposure is <10%. A number of randomized clinical trials in the past decade have compared the outcomes of laparoscopic Heller myotomy to pneumatic dilation and to botulinum toxin injection. In each of these trials, laparoscopic Heller myotomy and partial fundoplication was superior to the alternative treatment. Lastly, a randomized clinical trial examining the need for fundoplication following Heller myotomy demonstrated a great deal more reflux in patients without fundoplication, and no better swallowing in the Heller-only group. The best treatment for achalasia is a laparoscopic Heller myotomy and partial fundoplication. Esophageal Resection for End-Stage Motor Disorders of the Esophagus Patients with dysphagia and long-standing benign disease, whose esophageal function has been destroyed by the disease process or multiple previous surgical procedures, are best managed by esophagectomy. Fibrosis of the esophagus and cardia can result in weak contractions and failure of the distal esophageal sphincter to relax. The loss of esophageal contractions can result in the stasis of food, esophageal dilatation, regurgitation, and aspiration. In these situations esophageal replacement is usually required to establish normal alimentation. Before proceeding with esophageal resection for patients with end-stage benign disease, the choice of the organ to substitute for the esophagus. The choice of replacement is affected by a number of factors, as described later in the section on Techniques of Esophageal Reconstruction. If minimally invasive esophagectomy is to be performed, thoracoscopic dissection should be combined with abdominal dissection. Its incidence is highly variable, ranging from approximately 20 per 100,000 in the United States and Britain, to 160 per 100,000 in certain parts of South Africa and the Honan Province of China, and even 540 per 100,000 in the Guriev district of Kazakhstan. The environmental factors responsible for these localized high-incidence areas have not been conclusively identified, though additives to local foodstuffs (nitroso compounds in pickled vegetables and smoked meats) and mineral deficiencies (zinc and molybdenum) have been suggested. In Western societies, smoking and alcohol consumption are strongly linked with squamous carcinoma. Other definite associations link squamous carcinoma with longstanding achalasia, lye strictures, tylosis (an autosomal dominant disorder characterized by hyperkeratosis of the palms and soles), and human papillomavirus. Once a nearly uniformly lethal disease, survival has improved slightly because of advances in the understanding of its molecular biology, screening and surveillance practices, improved staging, minimally invasive surgical techniques, and neoadjuvant therapy. It now occurs not only considerably more frequently, but in younger patients, and is often detected at an earlier stage. These facts support rethinking the traditional approach of assuming palliation is appropriate in all patients. The historical focus on palliation of dysphagia in an elderly patient with comorbidities should change when dealing with a young patient with dependent children and a productive life ahead. Rarely, it arises in the submucosal glands, and forms intramural growths that resemble the mucoepidermal and adenoid cystic carcinomas of the salivary glands. This risk is similar to the risk for developing lung cancer in a person with a 20-pack-per-year history of smoking. Extension of the primary tumor into the tracheobronchial tree can occur primarily with squamous cell carcinoma and can cause stridor, tracheoesophageal fistula and resultant coughing, choking, and aspiration pneumonia. Rarely, severe bleeding from the primary tumor or from erosion into the aorta or pulmonary vessels occurs. In these communities, the most prominent early symptom is pain on swallowing rough or dry food. In patients that present with back pain at the time of esophageal cancer diagnosis, there is usually distant metastasis or celiac encasement. Dysphagia usually presents late in the natural history of the disease, because the lack of a serosal layer on the esophagus allows the smooth muscle to dilate with ease. As a result, the dysphagia becomes severe enough for the patient to seek medical advice only when more than 60% of the esophageal circumference is infiltrated with cancer. Tracheoesophageal fistula may be present in some patients on their first visit to the hospital, and more than 40% will have evidence of distant metastases.
Because of the length of esophageal involvement erectile dysfunction youtube cheap apcalis sx 20mg otc, rigid dilators (Maloney or Savary) are often used. The endoscopic appearance of eosinophilic esophagitis is characteristically a series of stacked mucosal rings. They can be categorized into one or a combination of the following abnormalities: (a) inadequate oropharyngeal bolus transport; (b) inability to pressurize the pharynx; (c) inability to elevate the larynx; (d) discoordination of pharyngeal contraction and cricopharyngeal relaxation; and (e) decreased compliance of the pharyngoesophageal segment secondary to neuromuscular disease. The latter may result in incomplete relaxation of the cricopharyngeus and cervical esophagus during swallowing. Taken together, these disorders are termed transit dysphagia by many Transit dysphagia is usually congenital or results from acquired disease involving the central and peripheral nervous system. Pure muscular diseases such as radiation-induced myopathy, dermatomyositis, myotonic dystrophy, and myasthenia gravis are less common causes. Rarely, extrinsic compression of the cervical esophagus by thyromegaly, lymphadenopathy, or hyperostosis of the cervical spine can cause transit dysphagia. These are anatomic manifestations of neuromuscular disease, and result from the loss of muscle compliance in portions of the pharynx and esophagus composed of skeletal muscle. Careful analysis of video- or cineradiographic studies combined with manometry using specially designed catheters can identify the cause of a pharyngoesophageal dysfunction in Diagnostic Assessment of the Cricopharyngeal Segment. Transit dysphagia difficult to assess with standard manometric techniques because of the rapidity of the oropharyngeal phase of swallowing, the elevation of the larynx, and the asymmetry of the cricopharyngeus. Note its marked enlargement and evidence of laryngeal inlet aspiration on recent esophagogram. Schematic drawing of a pharyngeal pressure wave indicating the presence of the bolus pressure. Schematic drawing of the manometric recording typically seen during cricopharyngeal sphincter relaxation. Motility studies may demonstrate inadequate pharyngeal pressurization, insufficient or lack of cricopharyngeal relaxation, marked discoordination of pharyngeal pressurization, cricopharyngeal relaxation and cervical esophageal contraction, or a hypopharyngeal bolus pressure suggesting decreased compliance of the skeletal portion of the cervical esophagus. The abnormality most apt to be present is a loss of compliance in the pharyngoesophageal segment manifested by an increased bolus pressure. Cook and colleagues have demonstrated an increased resistance to the movement of a bolus through what appears on manometry to be a completely relaxed cricopharyngeal sphincter. Using simultaneous manometry and videofluoroscopy, they showed that, in these patients, the cricopharyngeus is only partially relaxed; that is, the sphincter is relaxed enough to allow a drop of its pressure to esophageal baseline on manometry, but insufficiently relaxed to allow unimpaired passage of the bolus into the esophagus. Increasing the diameter of this noncompliant segment reduces the resistance imposed on the passage of a bolus. These findings correlate well with the observation of a decreased compliance of the upper esophagus demonstrated by videoradiography and the findings on detailed manometric studies of the pharynx and cervical esophagus. They suggest that the diverticulum develops as a consequence of the outflow resistance to bolus transport through the noncompliant muscle of the pharyngoesophageal segment. Pharyngoesophageal diverticula have been reported to occur in 1 of 1000 routine barium examinations, and classically occur in elderly, white males. Cross-section of the neck at the level of the thyroid isthmus that shows the surgical approach to the hypopharynx and cervical esophagus. Presenting symptoms include dysphagia associated with the spontaneous regurgitation of undigested, bland material, often interrupting eating, or drinking. On occasion, the dysphagia can be severe enough to cause debilitation and significant weight loss. Chronic aspiration and repetitive respiratory infection are common associated complaints. Endoscopy is usually difficult in the presence of a cricopharyngeal diverticulum, and potentially dangerous, owing to obstruction of the true esophageal lumen by the diverticulum and the attendant risk of diverticular perforation. The low morbidity and mortality associated with cricopharyngeal and upper esophageal myotomy have encouraged a liberal approach toward its use for almost any problem in the oropharyngeal phase of swallowing. This attitude has resulted in an overall success rate in the relief of symptoms of only 64%. When patients are selected for surgery using radiographic or motility markers of disease, a much higher proportion will benefit. Two methods of cricopharyngoesophageal myotomy are in common use, one using traditional surgical approaches, and one using rigid laryngoscopy and a linear cutting stapler.
The portal vein drains the splanchnic blood from the stomach best erectile dysfunction doctors nyc order 20 mg apcalis sx with amex, pancreas, spleen, small intestine, and majority of the colon to the liver before returning to the systemic circulation. The portal vein pressure in an individual with normal physiology is low at 3 to 5 mmHg. The portal vein is valveless, however, and in the setting of portal hypertension, the pressure can be quite high (20 to 30 mmHg). This results in decompression of the systemic circulation through portocaval anastomoses, most commonly via the coronary (left gastric) vein, which produces esophageal and gastric varices with a propensity for major hemorrhage. Another branch of the main portal vein is the superior pancreaticoduodenal vein (which comes off low in an anterior lateral position and is divided during pancreaticoduodenectomy). Closer to the liver, the main portal vein typically gives off a short branch (posterior lateral) to the caudate process on the right side. It is important to identify this branch and ligate it during hilar dissection for anatomic right hemihepatectomy to avoid avulsion. The portal vein is formed by the confluence of the splenic and superior mesenteric veins. The coronary (left gastric) vein drains into the portal vein in the vicinity of the confluence. This can be a source of torrential bleeding if control of it is lost during right hepatectomy. The hepatic vein branches bisect the portal branches inside the liver parenchyma. The cystic duct itself also has a variable pattern of drainage into the common bile duct. This can lead to potential injury or postoperative bile leakage during cholecystectomy or hepatic resection, and the surgeon needs to expect these variants. Neural Innervation and Lymphatic Drainage Bile Duct and Hepatic Ducts Within the hepatoduodenal ligament, the common bile duct lies anteriorly and to the right. It gives off the cystic duct to the gallbladder and becomes the common hepatic duct before dividing into the right and left hepatic ducts. In general, the hepatic ducts follow the arterial branching pattern inside the liver. The right anterior hepatic duct usually enters the liver above the hilar plate, whereas the right posterior duct dives behind the right portal vein and can be found on the surface of the caudate process before entering the liver. The left hepatic duct typically has a longer extrahepatic course before giving off segmental branches behind the left portal vein at the base of the umbilical fissure. Considerable variation exists, and in 30% to 40% of the parasympathetic innervation of the liver comes from the left vagus, which gives off the anterior hepatic branch, and the right vagus, which gives off the posterior hepatic branch. The sympathetic innervation involves the greater thoracic splanchnic nerves and the celiac ganglia, although the function of these nerves is poorly understood. The denervated liver after hepatic transplantation seems to function with normal capacity. As described by Couinaud in 1957, the bifurcation of the hepatic ducts has a variable pattern in approximately 40% of cases. This is particularly important for resection of hilar cholangiocarcinoma, which has a high incidence of lymph node metastases. One crucial role is the processing of absorbed nutrients through the metabolism of glucose, lipids, and proteins. The liver maintains glucose concentrations in a normal range over both short and long periods by performing several important roles in carbohydrate metabolism. In the fasting state, the liver ensures a sufficient supply of glucose to the central nervous system. The liver can produce glucose by breaking down glycogen through glycogenolysis and by de novo synthesis of glucose through gluconeogenesis from noncarbohydrate precursors such as lactate, amino acids, and glycerol. In the postprandial state, excess circulating glucose is removed by glycogen synthesis or glycolysis and lipogenesis.
Recently impotence hernia buy apcalis sx now, Y-graft approaches to aortic arch repair have been introduced71 that essentially debranch the brachiocephalic vessels and move them forward. Illustration of our current valve-sparing procedure for replacing the aortic root and ascending aorta for treatment of A. The ascending aorta is opened after cardiopulmonary bypass and cardioplegic arrest are established and the distal ascending aorta is clamped. Buttons of surrounding tissue are used to mobilize the origins of the coronary arteries. After the distal anastomosis is completed, six sutures reinforced with Teflon pledgets are placed in the plane immediately below the aortic valve annulus. The subannular sutures are placed through the base of a synthetic aortic root graft, which is then is parachuted down around the valve. After the root graft is cut to an appropriate length, the valve commissures and leaflets are positioned within the graft. The button surrounding the origin of the left main coronary artery is sewn to an opening cut in the root graft. The button surrounding the origin of the right coronary artery is sewn to an opening cut in the root graft. The completed valve-sparing aortic root replacement and graft repair of the ascending aorta is shown. During a subsequent operation, this "trunk" is used to facilitate repair of the descending thoracic aorta through a thoracotomy incision. This technique permits access to the distal portion of the graft during the second operation without the need for dissection around the distal transverse aortic arch; this reduces the risk of injuring the left recurrent laryngeal nerve, esophagus, and pulmonary artery if an open approach is used at the second stage. Illustration of a modified Bentall procedure for replacing the aortic root and ascending aorta. The aortic valve and entire ascending aorta, including the sinuses of Valsalva, have been replaced by a mechanical composite valve graft. The coronary arteries with buttons of surrounding aortic tissue have been mobilized and are being reattached to openings in the aortic graft. Cardiopulmonary Bypass Perfusion Strategies Like the operations themselves, perfusion strategies used during proximal aortic surgery depend on the extent of the repair. Aneurysms that are isolated to the ascending segment can be replaced by using standard cardiopulmonary bypass and distal ascending aortic clamping. This provides constant perfusion of the brain and other vital organs during the repair. Aneurysms involving the transverse aortic arch, however, cannot be clamped during the repair, which necessitates the temporary withdrawal of cardiopulmonary bypass support; this is called circulatory arrest. To protect the brain and other vital organs during the circulatory arrest period, hypothermia must be initiated before pump flow is stopped. Nonetheless, although brief periods of circulatory arrest generally are well tolerated, even this recently modified technique continues to have substantial limitations; as the duration of circulatory arrest increases, the well-recognized risks of brain injury and death increase dramatically. Additionally, some authors have raised the concern that reducing the degree of hypothermia narrows the safety margin that deep hypothermia provides, because it increases the risk of ischemic complications involving the spinal cord, kidneys, and other organs that now receive less hypothermic protection. Retrograde cerebral perfusion involves directing blood from the cardiopulmonary bypass circuit into the brain through the superior vena cava. Upon initiation, cold blood is delivered into the brain via the right common carotid artery. Note that, with this technique, blood flow to the left side of the brain requires an intact circle of Willis. The unique anatomy of the aortic arch and the need for uninterrupted cerebral perfusion pose difficult challenges. There are reports of the use of "homemade" grafts to exclude arch aneurysms; however, these grafts are highly experimental at this time. For example, in 1999, Inoue and colleagues81 reported placing a triple-branched stent graft in a patient with an aneurysm of the aortic arch. The three brachiocephalic branches were positioned by placing percutaneous wires in the right brachial, left carotid, and left brachial arteries. The patient underwent two subsequent procedures: surgical repair of a right brachial pseudoaneurysm and placement of a distal stent graft extension to control a major perigraft leak. Buy apcalis sx 20 mg cheap. Erectile Dysfunction.wmv.
|