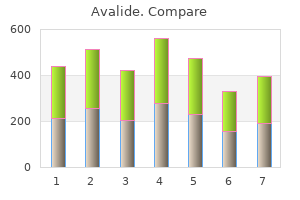
Avalide"Buy avalide 162.5mg on-line, arrhythmia medication list". By: G. Myxir, MD Clinical Director, Ohio University Heritage College of Osteopathic Medicine The goals of surgical management of diverticular disease include controlling sepsis blood pressure stages purchase 162.5 mg avalide with visa, eliminating com plications such as fistula or obstruction, removing the diseased colonic segment, and restoring intestinal continuity. These goals must be obtained while minimiz ing morbidity rate, length of hospitalization, and cost in addition to maximizing survival and quality of life. Table 19-3 lists the operations most commonly indicated based upon Hinchey classification and the predicted morbidity and mortality rates. Surgical objec tives include removal of the diseased sigmoid down to the rectosigmoid junction. The current options for uncom plicated diverticular disease include an open sigmoid resection or a laparoscopic sigmoid resection. Laparoscopic techniques have been employed for complicated diverticular disease; however, higher conversion rates to open techniques have been reported. Percutaneous drainage is recommended for abscesses 5 cm with a welldefined wall that is accessible. Con traindications to percutaneous drainage are no percu taneous access route, pneumoperitoneum, and fecal peritonitis. If the patient has significant comorbidities, making operative intervention risky, a limited procedure including intraoperative peritoneal lavage (irrigation), omental patch to the oversewn perforation, and proxi mal diversion of the fecal stream with either an ileos tomy or transverse colostomy can be performed. A limited approach to these patients is associated with a decreased mortality rate. It is often associated with a redundant sigmoid colon, pelvic laxity, and a deep rectovaginal septum (pouch of Douglas). Initially, rectal prolapse was felt to be the result of early internal rectal intussusception, which occurs in the upper to mid rectum. However, only 1 of 38 patients with internal prolapse followed for >5 years developed full-thickness prolapse. Recurrent diverticular disease develops in patients following inadequate surgical resection. Women with rectal prolapse have a higher incidence of associated pelvic floor disorders including urinary incontinence, rectocele, cystocele, and enterocele. Anatomy and pathophysiology Rectal prolapse (procidentia) is a circumferential, fullthickness protrusion of the rectal wall through the anal In external prolapse, the majority of patient complaints include anal mass, bleeding per rectum, and poor perianal hygiene. Other associated findings include outlet obstruction (anismus) in 30%, colonic inertia in 10%, and solitary rectal ulcer syndrome in 12%. Office evaluation is best performed after the patient has been given an enema, which enables the prolapse to protrude. An important distinction should be made between full-thickness rectal prolapse and isolated mucosal prolapse associated with hemorrhoidal disease. Mucosal prolapse is known for radial grooves rather than circumferential folds around the anus and is due to increased laxity of the connective tissue between the submucosa and underlying muscle of the anal canal. If rectal prolapse is associated with chronic constipation, the patient should undergo a defecating proctogram and a sitzmark study. In colonic inertia, a sitzmark study will demonstrate retention of >20% of markers on abdominal x-ray 5 days after swallowing. Full-thickness prolapse associated with redundant rectosigmoid and deep pouch of Douglas (C, D, sagittal view). Transabdominal procedures can be performed effectively with laparoscopic techniques without increased incidence of recurrence. The goal of the transabdominal approach is to restore normal anatomy by removing redundant bowel and reattach ing the supportive tissue of the rectum to the presacral fascia. Colon resection, in gen eral, is reserved for patients with constipation and outlet obstruction. Previously, the presence of internal rectal prolapse identified on imaging studies has been considered a nonsurgical disorder and biofeedback was recom mended. However, only onethird of patients will have successful resolution of symptoms from biofeedback. A circular stapling device is inserted through the anus; the internal prolapse is identified and ligated with the stapling device. Transabdominal approaches have been associated with lower recurrence rates, but some patients with signifi cant comorbidities are better served by a transperineal approach.
Vascular disturbances A frequent misconception blood pressure medication vitamin k buy avalide american express, despite abundant experience to the contrary, is that pain associated with intraabdominal vascular disturbances is sudden and catastrophic in nature. The pain of embolism or thrombosis of the superior mesenteric artery or that of impending rupture of an abdominal aortic aneurysm certainly may be severe and diffuse. Yet, just as frequently, the patient with occlusion of the superior mesenteric artery has only mild continuous or cramping diffuse pain for 2 or 3 days before vascular collapse or findings of peritoneal inflammation appear. Indeed, absence of tenderness and rigidity in the presence of continuous, diffuse pain in a patient likely to have vascular disease is quite characteristic of occlusion of the superior mesenteric artery. Abdominal wall Pain arising from the abdominal wall is usually constant and aching. Movement, prolonged standing, and pressure accentuate the discomfort and muscle spasm. Simultaneous involvement of muscles in other parts of the body usually serves to differentiate myositis of the abdominal wall from an intraabdominal process that might cause pain in the same region. A most important, yet often forgotten, dictum is that the possibility of intrathoracic disease must be considered in every patient with abdominal pain, especially if the pain is in the upper part of the abdomen. Systematic questioning and examination directed toward detecting myocardial or pulmonary infarction, pneumonia, pericarditis, or esophageal disease (the intrathoracic diseases that most often masquerade as abdominal emergencies) will often provide sufficient clues to establish the proper diagnosis. Diaphragmatic pleuritis resulting from pneumonia or pulmonary infarction may cause pain in the right upper quadrant and pain in the supraclavicular area, the latter radiation to be distinguished from the referred subscapular pain caused by acute distention of the extrahepatic biliary tree. The ultimate decision as to the origin of abdominal pain may require deliberate and planned observation over a period of several hours, during which repeated questioning and examination will provide the diagnosis or suggest the appropriate studies. In addition, apparent abdominal muscle spasm caused by referred pain will diminish during the inspiratory phase of respiration, whereas it is persistent throughout both respiratory phases if it is of abdominal origin. Palpation over the area of referred pain in the abdomen also does not usually accentuate the pain and in many instances actually seems to relieve it. Thoracic disease and abdominal disease frequently coexist and may be difficult or impossible to differentiate. Referred pain from the spine, which usually involves compression or irritation of nerve roots, is characteristically intensified by certain motions such as cough, sneeze, or strain and is associated with hyperesthesia over the involved dermatomes. Pain referred to the abdomen from the testes or seminal vesicles is generally accentuated by the slightest pressure on either of these organs. In certain instances, such as hyperlipidemia, the metabolic disease itself may be accompanied by an intraabdominal process such as pancreatitis, which can lead to unnecessary laparotomy unless recognized. C1 esterase deficiency associated with angioneurotic edema is often associated with episodes of severe abdominal pain. Black widow spider bites produce intense pain and rigidity of the abdominal muscles and back, an area infrequently involved in intraabdominal disease. Severe muscle spasm, as in the gastric crises of tabes dorsalis, is common but is either relieved or is not accentuated by abdominal palpation. The pain is made worse by movement of the spine and is usually confined to a few dermatomes. Normal stimuli such as touch or change in temperature may be transformed in to this type of pain, which is frequently present in a patient at rest. The demonstration of irregularly spaced cutaneous pain spots may be the only indication of an old nerve lesion underlying causalgic pain. Distention of the abdomen is uncommon, and the pain has no relationship to the intake of food. Pain arising from spinal nerves or roots comes and goes suddenly and is of a lancinating type. It may be caused by herpes zoster, impingement by arthritis, tumors, herniated nucleus pulposus, diabetes, or syphilis. It is not associated with food intake, Few abdominal conditions require such urgent operative intervention that an orderly approach need be abandoned, no matter how ill the patient. Under these circumstances, all obstacles must be swept aside, adequate venous access for fluid replacement obtained, and the operation begun. Avalide 162.5 mg amex. Water Fasting w/Vegan Diet Cures High Blood Pressure - Dr. Goldhamer. In general heart attack on plane best 162.5mg avalide, hemorrhage tends to occur before age 50 years, in patients with a family history of intracranial hemorrhage, and in those who have survived a previous bleed, have aneurysms >10 mm, and have uncontrolled hypertension. Cardiac valvular abnormalities occur in 25% of patients, most commonly mitral valve prolapse and aortic regurgitation. Although most valvular lesions are asymptomatic, some may progress over time and warrant valve replacement. Most patients are asymptomatic with normal liver function tests, but hepatic cysts may bleed, become infected, rupture, and cause pain. Although the frequency of liver cysts is equal between the sexes, women are more likely to have massive cysts. The three variants of nephronophthisis listed are the most prevalent of the currently described 11 forms of nephronophthisis. Abdominal wall and inguinal hernias also occur with a higher frequency than in the general population. Screening for asymptomatic intracranial aneurysms should be restricted to patients with a personal or family history of intracranial hemorrhage and those in high-risk occupations. A multidrug approach that includes agents to inhibit the renin-angiotensin system is frequently required. Lipid-soluble antimicrobials such as trimethoprimsulfamethoxazole and fluoroquinolones that have good cyst penetration are the preferred therapy for infected kidney and liver cysts. Pain management occasionally requires cyst drainage by percutaneous aspiration, sclerotherapy with alcohol, or, rarely, surgical drainage. Those undergoing kidney transplantation may require bilateral nephrectomy if the kidneys are massively enlarged or have been the site of infected cysts. Those with two truncating mutations frequently die shortly after birth, whereas those who survive beyond the neonatal period generally have at least one missense mutation. Up to 50% of affected neonates die of pulmonary hypoplasia, the result of oligohydramnios from severe intrauterine kidney disease. Impaired urinary concentrating ability and metabolic acidosis ensue as tubular function deteriorates. Longer-term survivors frequently develop complications of portal hypertension from periportal fibrosis. The diagnosis can be made in utero after 24 weeks of gestation in severe cases, but cysts generally become visible only after birth. The kidneys are enlarged, with small cysts, <5 mm, limited to the collecting tubules. Like the polycystins, fibrocystin has receptorlike features and may be involved in cell-cell and cell-matrix interactions. Improvements in neonatal intensive care, blood pressure management, dialysis, and kidney transplantation have led to survival in to adulthood. Although their precise functions are unclear, the defective protein products, named nephrocystins and inversin, localize to the primary cilium and associated basal body of renal epithelial cells, similar to the polycystins and fibrocystin. In the infantile form, the kidneys are large with histology similar to that of the juvenile form except that medullary cysts are more prominent and develop earlier. Salt and water replacement are required for patients with salt wasting and polyuria. Therapy should include sodium bicarbonate or citrate for acidosis, management of chronic kidney disease, and timely institution of dialysis and kidney transplantation. Two genetic loci have been defined, both with autosomal dominant transmission (Table 16-1). Impaired tubular function causes salt wasting and defective urinary concentration and acidification. Patients may present with polyuria, polydipsia, volume depletion, or systemic acidosis. Other abnormalities include blindness from amaurosis, oculomotor apraxia, cerebellar ataxia (Joubert syndrome), polydactyly, mental retardation, hepatic fibrosis, and ventricular septal defect. The presence of either mutation produces uncontrolled proliferation in numerous tissues, including the kidneys, skin, central nervous system, and heart. They occur bilaterally, are often multiple, and are usually asymptomatic; however, they may cause spontaneous bleeding, flank pain, hematuria, and life-threatening retroperitoneal hemorrhage.
Angiotensin and aldosterone also influence colonic absorption prehypertension quiz buy avalide 162.5mg mastercard, reflecting the common embryologic development of the distal colonic epithelium and the renal tubules. After food ingestion, the small intestine produces irregular, mixing contractions of relatively low amplitude, except in the distal ileum where more powerful contractions occur intermittently and empty the ileum by bolus transfers. IleocolonIc storage and salvage the distal ileum acts as a reservoir, emptying intermittently by bolus movements. There is increased appreciation of the intimate interaction between the colonic function and the luminal ecology. The resident bacteria in the colon are necessary for the digestion of unabsorbed carbohydrates that reach the colon even in health, thereby providing a vital source of nutrients to the mucosa. In health, the ascending and transverse regions of colon function as reservoirs (average transit, 15 h), and the descending colon acts as a conduit (average transit, 3 h). The colon is efficient at conserving sodium and water, a function that is particularly important in sodium-depleted patients in whom the small intestine alone is unable to maintain sodium balance. Diarrhea or constipation may result from alteration in the reservoir function of the proximal colon or the propulsive function of the left colon. Constipation may also result from disturbances of the rectal or sigmoid reservoir, typically as a result of dysfunction of the pelvic floor, the anal sphincters, or the coordination of defecation. Thus, the colon can partially compensate for excess fluid delivery to the colon because of intestinal absorptive or secretory disorders. The predominant phasic contractions in the colon are irregular and nonpropagated and serve a "mixing" function. Voluntary relaxation of the external anal sphincter (striated muscle innervated by the pudendal nerve) in response to the sensation produced by distention permits the evacuation of feces; this evacuation process can be augmented by an increase in intraabdominal pressure created by the Valsalva maneuver. The initial phase (10 min) is mediated by the vagus nerve in response to mechanical distention of the stomach. The subsequent response of the colon requires caloric stimulation and is mediated at least in part by hormones. Two common conditions, usually associated with the passage of stool totaling <200 g/d, must be distinguished from diarrhea, because diagnostic and therapeutic algorithms differ. Fecal incontinence is the involuntary discharge of rectal contents and is most often caused by neuromuscular deFecatIon Tonic contraction of the puborectalis muscle, which forms a sling around the rectoanal junction, is important to maintain continence; during defecation, sacral parasympathetic nerves relax this muscle, facilitating the straightening of the rectoanal angle. A careful history and physical examination generally allow these conditions to be discriminated from true diarrhea. The remaining 10% or so are caused by medications, toxic ingestions, ischemia, and other conditions. Infectious agents Most infectious diarrheas are acquired by fecal-oral transmission or, more commonly, via ingestion of food or water contaminated with pathogens from human or animal feces. In the immunocompetent person, the resident fecal microflora, containing >500 taxonomically distinct species, are rarely the source of diarrhea and may actually play a role in suppressing the growth of ingested pathogens. Diarrhea closely following food consumption at a picnic, banquet, or restaurant may suggest infection with Salmonella, Campylobacter, or Shigella from chicken; enterohemorrhagic E. Individuals at risk for diarrhea include those with either primary immunodeficiency. Infectious diarrhea is one of the most frequent categories of nosocomial infections in many hospitals and long-term care facilities; the causes are a variety of microorganisms but most commonly C. The pathophysiology underlying acute diarrhea by infectious agents produces specific clinical features that may also be helpful in diagnosis (Table 6-2). Profuse, watery diarrhea secondary to small-bowel hypersecretion occurs with ingestion of preformed bacterial toxins, enterotoxin-producing bacteria, and enteroadherent pathogens.
|