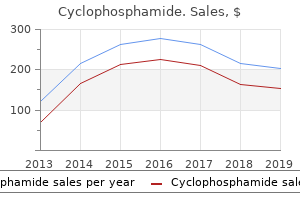
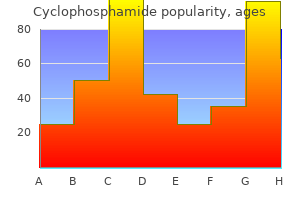
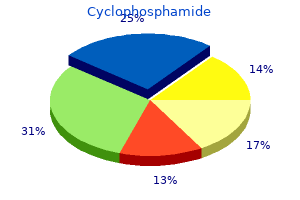
Cyclophosphamide"Cheap 50 mg cyclophosphamide fast delivery, symptoms of appendicitis". By: X. Kerth, M.A., M.D., Ph.D. Deputy Director, West Virginia University School of Medicine In very young in ants shakira medicine buy cyclophosphamide without prescription, Hyrtl ssure af ords a route o direct extension o in ection rom the middle ear to the subarachnoid spaces. Hyrtl ssure extends rom the subarachnoid space near the glossopharyngeal ganglion to the hypotympanum just in erior and anterior to the round window. Types of noise frequently used in clinical audiology are white noise (containing all frequencies in the audible spectrum at average equal amplitudes), narrow band noise (white noise with frequencies above and below a center frequency ltered out or reduced), and speech noise (white noise with frequencies > 3000 and < 300 Hz reduced by a lter). Natural resonance of external auditory canal is 3000 Hz; of middle ear, 800 to 5000 Hz, mostly 1000 to 2000 Hz; of tympanic membrane, 800 to 1600 Hz; of ossicular chain, 500 to 2000 Hz. Its resonant frequency is approximately 2700 Hz but varies by individual ear canal. Middle Ear e middle ear is an air- lled space approximately 5/8 inch high (15 mm), 1/8 to 3/16 inch wide (2-4 mm), 1/4 inch deep, and 1 to 2 cm 3 in volume. As s the wave travels through the cochlea, it moves the basilar and tectorial membranes. Because these two membranes have di erent hinge points, this movement results in a "shearing" motion that bends the hair cell stereocilia. For every frequency there is a highly speci c place on the basilar membrane where hair cells are maximally sensitive to that frequency, the basal end for high frequencies, and the apical end for low frequencies. Frequency-selective neurons transmit the neural code from the hair cells through the auditory system. For multiple frequencies (complex sound), there are several points of traveling wave maxima, and the cochlear apparatus constantly tunes itself for best reception and encoding of each component frequency. However, the major factor is the periphery, where the cochlea acts as both a transducer and analyzer of input frequency and intensity. Fibers ascend to the nuclei of the lateral lemniscus in the pons and to the inferior colliculus in the midbrain. Tonotopic organization is largely maintained throughout the auditory pathway from the cochlea to the cortex. Not all neuronal tracts synapse with each auditory nucleus sequentially in a "domino" fashion but rather may encounter two to ve synapses. In addition to the various nuclei, there are a erent and e erent bers, all exerting a mutual in uence on one another. It would be an enormous task to examine all of the possible pathways, nuclei, and processing involved in this neural transmission. However these pathways, nuclei and processing are complex and still active areas of ongoing research. In addition, ambient noises are also stronger in the low frequencies, around 250 Hz. When the patient no longer hears the sound, the examiner listens to the fork to see whether the tone is still audible. Patients with normal hearing will stop hearing the sound at about the same time as the tester (normal Schwabach). Patients with sensorineural hearing loss will stop hearing the sound before the examiner (diminished Schwabach). Patients with conductive hearing loss will hear the sound longer than the examiner (prolonged Schwabach).
Ectasia and fusiform enlargement of intracranial arteries are found in 3-5% of cases (12-14) treatment locator generic cyclophosphamide 50 mg online. Strokes with foci of restricted diffusion and subarachnoid hemorrhage may occur as complications of the underlying vasculopathy. A minority (approximately 10%) might be due to blood transfusions, other blood products given therapeutically, or organ/tissue transplantation. Pathology the most characteristic gross finding is generalized brain volume loss with symmetric enlargement of the ventricles and subarachnoid spaces. Multiple foci of microglia, macrophages, infiltration of microglial nodules, and multinucleated giant cells containing viral particles are typical. Patchy myelin pallor Other Congenital Infections Rubella (German Measles) Humans are the only reservoir for the rubella virus. Infection, Inflammation, and Demyelinating Diseases 344 Prior to widespread implementation of measles-mumpsrubella vaccine, epidemics of rubella occurred globally in 6- to 9-year intervals. Late infection causes generalized brain volume loss, dystrophic calcifications, and regions of demyelination and/or gliosis. Imaging findings are nonspecific, and, like other congenital infections, the timing of infection dictates the magnitude of destructive changes. Symptoms typically develop later in infancy with early signs and symptoms including jaundice, hepatosplenomegaly, and rash. Note prominent ventricles and sulci as well as multifocal white matter hyperintensities. Congenital, Acquired Pyogenic, and Acquired Viral Infections nose deformity, frontal bossing, rhagades (scars around the mouth and nose), Hutchinson teeth, seizures, stroke, and signs of increased intracranial pressure. Cisternal exudative meningitis can as a result of gumma formation lead to hypothalamic and pituitary dysfunction. Congenital varicella infection prior to 20 postconceptional weeks may lead to spontaneous abortion or embryopathic insults, including microcephaly secondary to cerebral destruction, chorioretinitis, limb and digit hypoplasia, and a distinctive pattern of skin scarring known as cicatrix. Imaging findings in congenital varicella zoster infection include microcephaly, parenchymal calcifications, ventriculomegaly, polymicrogyria, and nonpatterned necrosis of white matter, lobar cortical and subcortical tissues, and deep gray nuclei. Similar necrotic lesions have been described in the cerebellum, leading to cerebellar atrophy (12-17). The neonate may present with a sepsis-like illness, rash, fever, irritability, and seizures. Imaging findings in perinatal parechovirus infection include detection of bilateral confluent white matter abnormalities. These leukotropic changes have been mistaken for perinatal white matter hypoxic ischemic injury in the preterm newborn. Congenital Human Parvovirus B19 Human Parvovirus B19 is one well-documented cause of severe fetal anemia and a known cause of fetal death. The virus is also known to affect patients with immunologic disorders such as sickle cell anemia. The risk of maternal to fetal transmission is greatest in the first and second trimesters. Infection, Inflammation, and Demyelinating Diseases 346 Acquired Pyogenic Infections Meningitis Meningitis is a worldwide disease that leaves up to half of all survivors with permanent neurologic sequelae. Despite advances in antimicrobial therapy and vaccine development, bacterial meningitis represents a significant cause of morbidity and mortality. Infants, children, and the elderly or immunocompromised patients are at special risk. In this section, we focus on the etiology, pathology, and imaging findings of this potentially devastating disease. Tuberculous meningitis is common in developing countries and in immunocompromised patients. Pachymeningitis involves the duraarachnoid; leptomeningitis affects the pia and subarachnoid spaces. Direct geographic extension from sinusitis, otitis, or mastoiditis is the second most common method of spread. Penetrating injuries and skull fractures (especially of the skull base) are rare but important causes of meningitis. Meningitis can also be acute lymphocytic (viral) or chronic (tubercular or granulomatous). Group B-hemolytic streptococcal meningitis is the leading cause of newborn meningitis in developed countries, whereas enteric, gramnegative organisms (typically Escherichia coli, less commonly Enterobacter or Citrobacter) cause the majority of cases in developing countries. Ischemic strokes can be caused by vasospasm medicine 9 minutes discount cyclophosphamide 50mg mastercard, cocaineinduced vasoconstriction, vasculitis, or thrombosis (30-27). Bilateral globus pallidus infarction has also been reported as a stroke subtype in cocaine abuse. Toxic Encephalopathy Opioids and Derivatives the ten drugs most frequently involved in overdose deaths include several opioids: heroin, oxycodone, methadone, morphine, hydrocodone, and fentanyl. In addition to the direct effects of opioids on the brain, impurities and additives may produce systemic pathology. Hypotension and anoxia may also complicate the clinical and imaging appearance of opioid toxicity. Globus pallidus ischemia, very similar to that seen in carbon monoxide poisoning, is common. The freebase form is heated over aluminum foil and the vapors inhaled ("chasing the dragon"). Endocarditis is common and may result in septic emboli, brain abscesses, and vasculitis with mycotic aneurysm formation. Stimulation of opioid receptors in vascular smooth muscle may cause reversible vasospasm. Immune-mediated response to additives in injected heroin may cause ischemia or vasculitis. Pathology Autopsied brains of patients with heroin-associated encephalopathy show a sponge-like appearance of the cerebral white matter. Because the cerebellum has a high density of opioid receptors, similar changes can be seen in its white matter. The posterior cerebral white matter, posterior limb of the internal capsule, and globi pallidi are also commonly affected. There is often selective symmetric involvement of the posterior limb of the internal capsule, the corticospinal tract, the medial lemniscus, and the tractus solitarius (30-30). Confluent hyperintensity in the cerebral white matter, including the corpus callosum, is common in severe cases of heroin vapor encephalopathy (3031). Scattered multifocal hyperintensities in the subcortical or periventricular white matter are common but neither as prevalent nor as severe as seen with cocaine vasculopathy. Longer duration of heroin use is also associated with more damaging effects on brain functions. Oxycodone Imaging in the few reported cases of oxycodone and OxyContin overdose shows restricted diffusion in the cerebellar hemispheres and globi pallidi (30-32). A postopioid delayed toxic leukoencephalopathy similar to that caused by inhaled heroin has been reported with methadone. In contrast to heroin toxicity, cerebellar and brainstem changes are subtle or absent in adults. Accidental ingestion of methadone has been reported to cause severe cerebellar edema with acute obstructive hydrocephalus in children (30-34). Inhaled Gases and Toxins Some drugs of abuse such as heroin have multiple potential routes of administration. Examples include toxins such as Toxic Encephalopathy carbon monoxide and drugs of abuse such as nitrous oxide. Inhaled vapors from volatile, intrinsically liquid agents include amyl nitrite ("poppers") and industrial solvents. Studies have shown that petrol sniffing is often the earliest inhaled drug used and increases both the likelihood and earlier use of other drugs. Note faint hyperintense rim, thin hypointense underlying rim, and central coagulative necrosis seen as mildly hyperintense lesions. In addition to bilateral globi pallidi and cerebral white matter, various sites such as the cerebral cortex, cerebellum, hippocampus, amygdala, corpus callosum splenium, and insula are often involved. A faint rim of hyperintensity caused by hemorrhage or coagulative necrosis may be present (30-37A). Bilateral globi pallidi hyperintensities as well as foci of restricted diffusion in the subcortical white matter are typical. Generic cyclophosphamide 50 mg with mastercard. HIV / AIDS Causes Symptoms Treatments & many more Identified Stages.
Symptoms o rapid growth symptoms of dehydration discount 50mg cyclophosphamide with amex, pain, or aerodigestive tract compromise may occur with advanced malignancy but more commonly are associated with benign disease. Physical examination o the thyroid gland: It is best to orient toward the thyroid through adjacent cartilaginous laryngeal re erence points. Once the thyroid cartilage notch is identi ed, the anterior ring o the cricoid can be easily ound. One thumbbreadth below the cricoid, the isthmus can be palpated on the underlying upper cervical trachea. When identi ying the isthmus in the midline or the bilateral thyroid Cha pter 33: Thyroid and Parathyroid Glands 621 lobes laterally, it is use ul to have the patient swallow in order to have the thyroid roll upward underneath the thumb. It is important to determine the rmness o the thyroid nodule and its mobility or xation to the adjacent laryngotracheal complex. All patients with thyroid lesions should have a vocal cord examination to assess vocal cord motion. It should be strongly emphasized that voice and swallowing can be normal in the setting o complete unilateral vocal cord paralysis. Excellent screening test to de nitively diagnose euthyroidism, hyperthyroidism, or hypothyroidism and is recommended in the initial evaluation o patients with a thyroid nodule. The assay is inter ered with by antithyroglobulin antibodies that occur in approximately 15% to 25% o patients. Extensive overlap in thyroglobulin levels exists between benign thyroid conditions and thyroid carcinoma. Calcitonin, because o the rarity o medullary carcinoma o the thyroid, is not thought to be a reasonable routine screening test in patients with a solitary nodule. Ninety- ve percent o all nodules are typically ound to be cold; only 10% to 15% o cold nodules are malignant. T yroid scanning does not make it possible to separate nodules into benign and malignant categories. Ultrasonography It is recommended that thyroid sonography should be per ormed in all patients with one or more suspected thyroid nodules. Ultrasonography does not distinguish benign rom malignant lesions, but it can provide an accurate baseline. A sonogram can identi y the number, size, and shape o cervical nodes surrounding and distant rom the thyroid. Concerning ultrasound eatures o lymph nodes suggestive or malignancy include microcalci cations, irregular borders, hypervascularity, and loss o the lymph node hilum. Sonography may also be use ul in screening the thyroid or small lesions in patients presenting with metastatic thyroid cancer and or the evaluation o the thyroid in patients with a history o head and neck radiation. Indeterminate: I suspect carinoma then surgery; i suspect neoplasia then consier I123, hot nodules are ollowed, cold nodules should proceed to surgery. Benign nodules not easily palpated should be ollowed with U/S at the same ollow-up intervals. Cysts less than 4 cm can be aspirated and potentially suppressed, with surgery reserved or recurrent cyst ormation. Repeated nondiagnostic aspirates o cystic nodules need close observation or surgical excision. Nodules ound to be benign on cytology do not require urther diagnostic studies or treatment. Management guidelines or patients with thyroid nodules and di erentiated thyroid cancer. Medullary carcinoma o the thyroid can have a variety o histologic and cytologic orms. In order to de nitively di erentiate ollicular adenoma rom ollicular carcinoma, histologic evaluation o the entire capsule is necessary.
Approximately 80% of pseudoaneurysms affecting the carotid and vertebral arteries are extracranial symptoms nervous breakdown buy generic cyclophosphamide 50 mg online, whereas 20% involve their intracranial segments. Surgery and radiation therapy (typically for head and neck cancers) usually affect the extracranial carotid artery (carotid "blow- Etiology Pseudoaneurysms are usually caused by a specific inciting event-e. Nontraumatic Hemorrhage and Vascular Lesions 146 (6-33) Graphic depicts blood blister-like aneurysm, seen here as a broad-based hemispheric bulge covered with a tissue-paperthin layer of adventitia. Most pseudoaneurysms distal to the circle of Willis are infectious (mycotic), drug-related, neoplastic (oncotic), or traumatic. Traumatic pseudoaneurysms can form when the pericallosal artery is impacted against the inferior (free) margin of the falx cerebri during closed head injury (6-32). Pseudoaneurysms are purplish masses typically contained only by thinned, discontinuous adventitia and organized hematoma. Hematomas associated with pseudoaneurysms are often large and may contain clots of varying ages. Mycotic and oncotic pseudoaneurysms show extensive infiltration of the vessel wall by inflammatory or neoplastic cells, respectively. The parent vessel lumen is often occluded by thrombus, tumor, debris, or purulent exudate. The interval between the initial injury and neurologic deterioration varies from a few days up to several months. The major clinical presentations include sudden headache, loss of consciousness, recurrent epistaxis, and cranial nerve palsies. Patients with pseudoaneurysms distal to the circle of Willis often have a history of severe trauma (with or without skull fracture), systemic infection, or drug abuse. Findings suggestive of cerebral pseudoaneurysm include unexplained enlargement of an existing parenchymal hematoma. In the appropriate clinical setting, unusual or delayed evolution of hematoma also suggests the possibility of an underlying pseudoaneurysm. Intravascular enhancement represents the slow, delayed filling and emptying often seen with pseudoaneurysms. Digital subtraction angiography shows a globular, fusiform, or irregularly shaped "neckless" aneurysm with delayed filling and emptying of contrast agent (6-31B). Endovascular occlusion with a flow-diverting stent is now the method of choice to treat most intracranial pseudoaneurysms. Surgical options include trapping or sacrificing the parent artery with or without bypass graft. Dissecting aneurysm most frequently occurs in the posterior circulation, where the vertebral artery is the most common site. Fusiform aneurysm is also more common on the posterior circulation and typically involves the basilar artery. If sufficient collateral circulation is present, trapping and occluding the parent vessel may be an option. If endovascular treatment is unsuccessful, wrapping and revascularization have been recommended as potential surgical options. They are also extremely fragile lesions that lack a definable neck and easily tear during surgical clipping. A slight irregularity or small focal hemispherical bulge of the arterial wall may be the only finding (6-35). Pathology Arteriectasis is common with advanced atherosclerosis of the cerebral arteries. Nontraumatic Hemorrhage and Vascular Lesions 150 loss of elastica and media are present. Slow, turbulent flow in the residual lumen causes complex, sometimes bizarre signal (6-37). The residual lumen can be seen as a rounded "flow void" surrounded by complex thrombus that varies from hypointense to hyperintense.
|