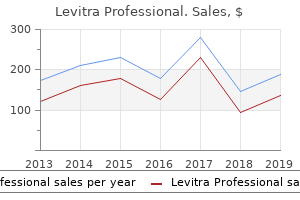
Levitra Professional"Order 20mg levitra professional visa, erectile dysfunction treatment penile prosthesis surgery". By: Z. Hamil, M.B.A., M.D. Assistant Professor, Lewis Katz School of Medicine, Temple University Basement Membrane erectile dysfunction treatment in delhi purchase levitra professional once a day, Lamina Propria, and Submucosa A thick "basement membrane" is characteristic of tracheal epithelium. At their free surface, they contain numerous cilia that, together, give the surface a brush-like appearance. This is owing to the linear aggregation of structures referred to as basal bodies, located at the proximal end of each cilium. Although basement membranes are not ordinarily seen in H&E preparations, a structure identified as such is seen regularly under the epithelium in the human trachea. Located beneath the tracheal epithelium is a distinctive layer typically referred to as a basement membrane. It usually appears as a glassy or homogeneous light-staining layer approximately 25 to 40 m thick. Electron microscopy reveals that it consists of densely packed collagenous fibers that lie immediately under the epithelial basal lamina. Structurally, it can be regarded as an unusually thick and dense reticular lamina and, as such, is part of the lamina propria. The Clara cell, as illustrated here, is interposed between the brush cell and the small granule cell. Adjacent, is the brush cell containing blunt microvilli, which are distinctive features of this cell. Cytoplasm of the brush cell shows a Golgi apparatus, lysosomes, mitochondria, and glycogen inclusions. This cell contains small secretory vesicles, most of which are in the basal portion of the cell. Lymphatic tissue, in both diffuse and nodular forms, is consistently present in the lamina propria and submucosa of the tracheal wall. It is also present in other parts of the respiratory system involved primarily with air conduction. Where the lamina propria ends, the elastic material is more extensive, and in specimens stained for these fibers, a distinct band of elastic material is seen. This band or elastic membrane marks the boundary between the lamina propria and submucosa. The submucosa is unlike that of most other organs, in which this connective tissue typically has a dense character. In the trachea, the submucosa is a relatively loose connective tissue similar in appearance to the lamina propria, which makes it difficult to determine where it begins. Diffuse lymphatic tissue and lymphatic nodules characteristically extend into this layer from the lamina propria. The submucosa contains the larger distributing vessels and lymphatics of the tracheal wall. Submucosal glands composed of mucus-secreting acini with serous demilunes are also present in the submucosa. Their ducts consist of a simple cuboidal epithelium and extend through the lamina propria to deliver their product, largely glycoproteins, on the epithelial surface. The glands are especially numerous in the cartilage-free gap on the posterior portion of the trachea. Some penetrate the muscle layer at this site and, therefore, also lie in the adventitia. The submucosal layer ends where its connective tissue fibers blend with the perichondrium of the cartilage layer. The tracheal cartilages, which number about 16 to 20 in humans, represent the next layer of the tracheal wall. They sometimes anastomose with adjacent cartilages, but their arrangement provides flexibility to the tracheal pipe and also maintains patency of the lumen. The adventitia, the outer layer, lies peripheral to the cartilage rings and trachealis muscle. It binds the trachea to adjacent structures in the neck and mediastinum and contains the largest blood vessels and nerves that supply the tracheal wall, as well as the larger lymphatics that drain the wall.
The thicker outer leaflet of the urothelial plaque contains a crystalline array of hexagonally arranged 16-nm in diameter proteins that are composed of a family of transmembrane proteins called uroplakins erectile dysfunction doctors baton rouge purchase cheap levitra professional on-line. The smooth muscle of the urinary passages is mixed with connective tissue, so that it forms parallel bundles rather than pure muscular sheets. Peristaltic contractions of the smooth muscle move the urine from the minor calyces through the ureter to the bladder. Ureters Each ureter conducts urine from the renal pelvis to the urinary bladder and is approximately 24 to 34 cm long. The distal part of the ureter enters the urinary bladder and follows an oblique path through the wall of the bladder. Transitional epithelium (urothelium) lines the luminal surface of the wall of the ureter. The smooth muscle is arranged in three layers: an inner longitudinal layer, a middle circular layer, and an outer longitudinal layer (Plate 78, page 738). However, the outer longitudinal layer is present only at the distal end of the ureter. Approximately 85% of urinary tract infections are caused by uropathogenic Escherichia coli bacteria, which colonize the transitional epithelium. The initial adhesion to the epithelium allows the bacteria to gain a foothold on the epithelial surface, thus preventing them from being removed during micturition. This binding is mediated As the bladder distends with urine, the openings of the ureters are compressed, reducing the possibility of reflux of urine into the ureters. Contraction of the smooth muscle of the bladder wall also compresses the openings of the ureters into the bladder. This action helps prevent the spread of infection from the bladder and urethra, frequent sites of chronic infection (particularly in females), to the kidney. In the terminal portion of the ureters, a thick outer layer of longitudinal muscle is present in addition to the two listed above, particularly in the portion of the ureter that passes through the bladder wall. Most descriptions of the bladder musculature indicate that this longitudinal layer continues into the wall of the bladder to form a principal component of its wall. The smooth muscle of the bladder, however, is not as clearly separated into distinctive layers. In the male, the urethra serves as the terminal duct for both the urinary and genital systems. It contains three openings, two for the ureters (ureteric orifices) and one for the urethra (internal urethral orifice). The triangular region defined by these three openings, the trigone, is relatively smooth and constant in thickness, whereas the rest of the bladder wall is thick and folded when the bladder is empty and thin and smooth when the bladder is distended. These differences reflect the embryologic origins of the trigone and the rest of the bladder wall: the trigone is derived from the embryonic mesonephric ducts, and the major portion of the wall originates from the cloaca. Toward the opening of the urethra, the muscle fibers form the involuntary internal urethral sphincter, a ring-like arrangement of muscle around the opening of the urethra. The smooth muscle bundles of the detrusor muscle are less regularly arranged than that of the tubular portions of the excretory passages, and thus the muscle and collagen bundles are randomly mixed (Plate 79, page 740). Contraction of the detrusor muscle of the bladder compresses the entire organ and forces the urine into the urethra. The ejaculatory ducts of the genital system enter the posterior wall of this segment, and many small prostatic ducts also empty into this segment. Membranous urethra extends for about 1 cm from the apex of the prostate gland to the bulb of the penis. It passes through the deep perineal pouch of the pelvic floor as it enters the perineum. Skeletal muscle of the deep perineal pouch surrounding the membranous urethra forms the external (voluntary) sphincter of the urethra. This segment is lined with a stratified or pseudostratified columnar epithelium that resembles the epithelium of the genital duct system more than it resembles the epithelium of the more proximal portions of the urinary duct system.
This concept allows a description of the exocrine secretory function of the liver comparable to that of the portal lobule erectile dysfunction injection drugs levitra professional 20mg discount. The hepatocytes in each liver acinus are described as being arranged in three concentric elliptical zones surrounding the short axis. Zone 3 is farthest from the short axis and closest to the terminal hepatic vein (central vein). This zone corresponds to the most central part of the classic lobule that surrounds the terminal hepatic vein. On the other hand, cells in zone 3 are the first to show ischemic necrosis (centrilobular necrosis) in situations of reduced perfusion and the first to show fat accumulation. Normal variations in enzyme activity, the number and size of cytoplasmic organelles, and the size of cytoplasmic glycogen deposits are also seen between zones 1 and 3. Cells in zone 2 have functional and morphologic characteristics and responses intermediate to those of zones 1 and 3. Blood Vessels of the Parenchyma the blood vessels that occupy the portal canals are called interlobular vessels. Only the interlobular vessels that form the smallest portal triads send blood into the sinusoids. The larger interlobular vessels branch into distributing vessels that are located at the periphery of the lobule. The central vein courses through the central axis of the classic liver lobule, becoming larger as it progresses through the lobule and empties into a sublobular vein. Several sublobular veins converge to form larger hepatic veins that empty into the inferior vena cava. The structure of the portal vein and its branches within the liver is typical of veins in general. In addition to providing arterial blood directly to the sinusoids, the hepatic artery provides arterial blood to the connective tissue and other structures the zonation is important in the description and interpretation of patterns of degeneration, regeneration, and specific toxic effects in the liver parenchyma relative to the degree or quality of vascular perfusion of the hepatic cells. As a result of the sinusoidal blood flow, the oxygen gradient, metabolic activity of the hepatocytes, and distribution of hepatic enzymes vary across the three zones. The distribution of liver damage resulting from ischemia and exposure to toxic substances can be explained using this zonal interpretation. Cells in zone 1 are the first to receive oxygen, nutrients, and toxins from the sinusoidal blood and the first to show morphologic changes after bile duct occlusion (bile stasis). These cells are also the last to die if circulation is impaired and Kupffer cell blood flow bile duct portal vein hepatic artery Kupffer cell. Previously, they had been described as lying on the luminal surface of the endothelial cells. This schematic diagram of a part of a classic lobule shows the components of the portal triads, hepatic sinuses, terminal hepatic venule (central vein), and associated plates of hepatocytes. Note that the direction of bile flow (green arrows) is opposite that of the blood flow. Capillaries in these larger portal canals return the blood to the interlobular veins before they empty into the sinusoid. The central vein is a thin-walled vessel receiving blood from the hepatic sinusoids. The endothelial lining of the central vein is surrounded by small amounts of spirally arranged connective tissue fibers. The central vein, so named because of its central position in the classic lobule, is actually the terminal venule of the system of hepatic veins and, thus, is more properly called the terminal hepatic venule. The sublobular vein, the vessel that receives blood from the terminal hepatic venules, has a distinct layer of connective tissue fibers, both collagenous and elastic, just external to the endothelium. Because they are solitary vessels, they can be readily distinguished in a histologic section from the portal veins that are members of a triad. One hepatic sinusoid (top) displays a stellate sinusoidal macrophage (Kupffer cell). The remainder of the sinusoid as well as the other sinusoid is lined by thin endothelial cell cytoplasm. Surrounding each sinusoid is the perisinusoidal space (space of Disse), which contains numerous hepatocyte microvilli.
Note that the sensory hair processes of the cells are hardly discernable and are covered by the cupula erectile dysfunction consult doctor buy levitra professional canada. The underlying loose connective tissue extends to the wall of the bony labyrinth and contains nerve fibers with associated Schwann cells, fibroblasts, capillaries, and other connective tissue cells. This high-magnification view of the macula of the utricle shows sensory epithelium similar to that of the crista ampullaris. Sensory epithelium is overlaid by the otolithic membrane containing a darker stained layer of otoconia (otolithes) on its surface. The outer surface of the otolithic membrane lies opposite the surface in which the stereocilia of the hair cells are embedded. The otolithic membrane moves on the macula in a manner analogous to that by which the cupula moves on the crista. Stereocilia of the hair cells are deflected by gravity in the stationary individual when the otolithic membrane and its otoliths pull on the stereocilia. They are also displaced during linear movement when the individual is moving in a straight line and the otolithic membrane drags on the stereocilia because of inertia. Displacement of stereocilia in the opposite direction away from the kinocilium causes hyperpolarization of hair cells and inhibits generation of the action potential. The scala vestibuli and scala tympani are the spaces above and below, respectively, the scala media. As shown in this drawing, the macula of the utricle (as well as macula of the saccule) functions as a sensor for gravity and linear acceleration. For example, when the head of the individual shown in this diagram is tilted forward, tiny crystals of calcium carbonate called otoconia are shifted on the surface of the otolithic membrane. The hair cell processes are embedded in the gelatinous polysaccharide otolithic membrane. The luminal surface of the membrane is covered by otoconia that are heavier than endolymph. As visible on the map below the macula, the hair cells are polarized with respect to the striola, an imaginary plane that curves through the center of each macula. Note that on each side of the striola, the kinocilia of the hair cells are oriented in opposite directions facing toward the striola (see direction of the blue and green arrows on the polarization map of the utricle). This arrangement is only seen in the utricle because in the macula of the saccule, the kinocilia of the hair cells are turned away from the striola. The scala vestibuli and the scala tympani are perilymph-containing spaces that communicate with each other at the apex of the cochlea through a small channel called the helicotrema. The scala vestibuli begins at the oval window, and the scala tympani ends at the round window. The scala media is a triangular space with its acute angle attached to the modiolus. In transverse section, the scala media appears as a triangular space with its most acute angle attached to a bony extension of the modiolus, the osseous spiral lamina. The lateral or outer wall of the scala media is bordered by a unique epithelium, the stria vascularis. Cross-section of the basal turn of the cochlear duct is shown in the box on the smaller orientation view. This view of a mid-modiolar section of the cochlea illustrates the position of the cochlear duct within the 2. Observe that at the top of the cochlea, scala vestibuli and scala tympani communicate with each other at the helicotrema. The scala media and the osseous spiral lamina divide the cochlea into the scala vestibuli and the scala tympani, which are filled with perilymph. The scala media (the space within the cochlear duct) is filled with endolymph and contains the organ of Corti. The axons of the spiral ganglion cells form the cochlear part of the vestibulocochlear nerve. Two cell types can be observed: a mesothelial cell, which faces the scala vestibuli and is bathed by perilymph, and an epithelial cell, which faces the scala media and is bathed by endolymph. Cheap levitra professional amex. Fish Oil Cures Erectile Dysfunction – How To Cure Erectile Dysfunction Naturally.
|